- if you have a symptom of periodontal disease, like gum bleeding, gum swelling or tooth mobility
- if your parents or siblings have periodontitis and you worry that it can be inherited
- if you want to cover the exposed roots with gums, when your gums have receded and the teeth look long
- if you feel bad about your teeth because they are too short or you have a gummy smile
- if you are interested in replacing missing teeth with dental implants
- if you are interested in placing implants to provide extra support to your denture
- if you are planning on getting pregnant or you already are and you wish to get informed about “pregnancy gingivitis” or for recent data concerning the association between periodontitis and pregnancy complications
- if you suffer from some sort of cardiovascular disease. Recent research has demonstrated that periodontal disease is associated to atherosclerotic diseases
- if you suffer from diabetes. Recent research has shown that periodontal disease can destabilize your blood sugar levels which, in turn, can exacerbate your periodontal condition

Then, because we consider as a very important issue that the patient comprehends completely his/her periodontal condition, we are more than willing to dedicate as time as needed to explain the problem in a simple and comprehensive manner. We will answer, responsibly, to all of your questions and we will set realistic objectives for your treatment depending on the prognosis of each tooth.
Through this way, based on the diagnosis and your expectations, we are going to suggest one or more alternative treatment plans.
Our aim is that, at the end of the session, you have understood completely your periodontal condition and the treatment plan required, in order for you to regain your good oral health and the healthy smile you desire.

- Patient suffering from gingivitis
Gingivitis is easily treated at the dental office through the procedure of scaling (teeth cleaning). The maintenance of the healthy status of the gingiva, after treatment, requires daily and effective oral hygiene (brushing-flossing) by the patient as well as regular re-examinations (recalls).
However, there are also some other factors which can’t cause gingivitis by themselves, but may contribute to the exacerbation of inflammation when they coexist with dental plaque. Such factors are:
- smoking
- specific medications
- hormonal disorders during puberty, pregnancy or menopause
- heredity
- stress and anxiety
- carious lesions, and former crowns or bridges that don’t fit properly and promote the retention of bacteria
If gingivitis is not treated on time, it may progress to periodontitis which is more destructive.
Plaque and tartar are removed with special scalers and ultrasound tools. This process is called scaling, commonly known as “simple teeth cleaning”. It is painless and most of the times local anesthesia is not required. In this phase, ill-fitting fillings that promote plaque/tartar retention are replaced.


Additionally, as part of the treatment, meticulous oral hygiene instructions (use of toothbrush, floss or even antibacterial mouthwashes) are provided. Only through the effective oral hygiene the patient can prevent new plaque formation and preserve the healthy status of the gums in the long term.
Approximately one month after scaling the gingiva and the oral hygiene effectiveness are re-evaluated. If necessary, additional scaling takes place wherever needed. After therapy, the patient enters a re-call system and is periodically re-evaluated every 6-12 months, in order to avoid the recurrence of gingivitis.
Periodontitis is the progression of gingivitis. However, in contrast to gingivitis in periodontitis inflammation is not confined only in the gingiva (gums), but extends deeper affecting and destroying the bone of the jaw, which supports the teeth.
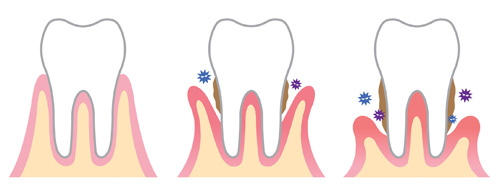
Periodontitis can affect some or all the teeth. The severity and the pace of tissue destruction varies from patient to patient. There are cases where the disease progresses rapidly, even in young people. However, most of the times, the destruction progresses in a slow pace and is more apparent in middle-aged or older individuals. If periodontitis remains untreated, the patient may lose his/her teeth due to the destruction of the jaw-bone that supports them.

Patient suffering from periodontitis
It is also notable, that although in peridontitis we counter the destruction of the bone around the teeth, patients, usually, do not have pain. Nevertheless, because of the weakening of the supportive system of the teeth, patients usually complain that their teeth have mobility and have migrated. Last but not least, due to the destruction of the bone, many times, the gingiva (gums) recede and the roots of the teeth get exposed. In such cases, empty spaces “black triangles” are created between the teeth and teeth look longer.
To sum up, the symptoms of periodontitis are:
- red and swollen gums
- gum bleeding when chewing
- tooth mobility
- tooth migration
- gum recession
- root exposure
- spaces between the teeth
Apart from bacteria, there are and some other factors which can’t cause gingivitis by themselves, but may contribute to the exacerbation of inflammation when they coexist with dental plaque. Such factors are:
- smoking
- specific medications
- hormonal disorders during puberty, pregnancy or menopause
- diabetes mellitus
- heredity
- stress and anxiety
- carious lesions, and former crowns or bridges that don’t fit properly and promote the retention of bacteria
Additionally, as part of the treatment, meticulous oral hygiene instructions (use of toothbrush, floss, inter-dental brushes, or even antibacterial mouthwashes) are provided. Only with effective oral hygiene the patient can prevent new plaque formation and preserve the healthy status of the gums in the long term.
Approximately 1 1/2 months after therapy the healing of the periodontal tissues and the oral hygiene effectiveness are re-evaluated. If necessary, additional scaling and root planing take place wherever needed. After therapy, the patient enters a re-call system and is periodically re-evaluated every 4-6 months, in order to avoid the recurrence of periodontitis.
Conservative treatment of periodontitis
Periodontitis is an inflammatory and destructive disease of the gingiva (gums) and of the jaw bone that supports the teeth. The destruction is irreversible which means that when periodontitis is treated full healing of the damaged tissues does not take place. Hence, while after treatment the tissues become healthy again and the progression of the disease is halted, the supportive bone that surrounds the teeth and was lost due to periodontitis is not regenerated.
It should be noted, that there are cases where, with the help of bone grafts we can rebuild part of the lost bone. However, these cases are scarce and their success largely depends on the morphology of the bone defect (see Bone grafts for more details).
The basic philosophy of the treatment is the removal of the causal factor of periodontitis, which is none other than the microbial plaque/tartar that accumulates on the surface of the teeth. After local anesthesia, the plaque and tartar found in the periodontal pockets are removed with special scalers and ultrasound tools and the surfaces of the contaminated roots are smoothened. This process is called scaling and root planing and is widely known as deep cleaning. It is painless, as it is performed under local anesthesia. Nevertheless, a minority of patients can develop the following days some sort of sensitivity to cold which is temporary and lasts around 2-3 weeks.
Scaling and root planning is completed in approximately 4 sessions. A quartile at a time, so as the process becomes more comfortable to the patient. In special cases, simultaneously to scaling and root planning, the use of antibiotics may be recommended. In this phase, ill-fitting fillings, that promote plaque/tartar retention, are replaced.
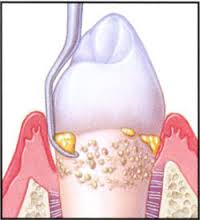 Scaling and root planing
Scaling and root planingAdditionally, as part of the treatment, meticulous oral hygiene instructions (use of toothbrush, floss, inter-dental brushes or even antibacterial mouthwashes) are provided. Only through the effective oral hygiene the patient can prevent plaque formation and preserve the healthy status of the periodontal tissues in the long term.
Approximately 1 1/2 months after scaling and root planning the periodontal tissues and the oral hygiene effectiveness are re-evaluated. If necessary, additional scaling and root planing take place wherever needed. After therapy, the patient enters a recall system and is periodically re-evaluated every 4-6 months, depending upon the case, in order to avoid the recurrence of periodontitis.
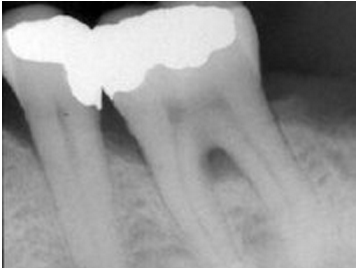
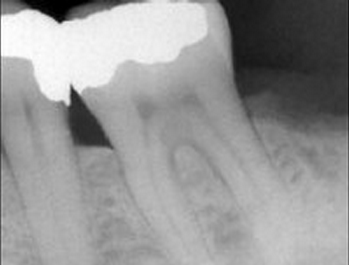
- Before treatment
- After treatment
Surgical treatment of periodontitis
Areas where the conservative periodontal therapy (scaling and root planning) was not effective are further treated surgically (open flap debridement). Many times, the deep pockets as well as the morphology of the multi-root teeth make the access for the debridement of the roots inadequate. This results in poor removal of the plaque/tartar from the root surfaces during the conservative phase of the treatment and therefore the preservation of inflammation.
Through periodontal surgery, the periodontist gains better access to those areas and removes effectively the plaque and tartar. Simultaneously, he can provide a new architecture to the gingiva and the underlying jaw bone, which will facilitate the patient to perform better oral hygiene and thus maintain the therapeutic effect.
The surgery is performed under local anesthesia and is completely painless. With a small incision in the gums, the periodontist reflects the gums from the teeth and obtains immediate access to the affected site. Inflamed tissues, plaque and calculus from the root surfaces are removed. Then, the gingiva and the bone are recontoured and the flaps are repositioned and secured with fine sutures. The sutures are removed after 1-2 weeks and at that time the healing process is evaluated.
The discomfort in the area is small (comparable to that of a tooth extraction), it usually lasts 1-3 days and is effectively treated with mild pain killers. In most cases, it is not necessary to prescribe antibiotics. During the first week of healing, the patient follows a soft diet and cleans the area through the use of a special mouthwash. After the first week and for another week the patient cleans the area with an extra soft toothbrush that is provided by the periodontist. After this healing period the patient’s diet and oral hygiene return to normal.
Upon completion of the surgical phase, periodic re-examinations follow, typically every 4-6 months to prevent recurrence of periodontitis.
Clearly, depending upon the case, the treatment of periodontitis may become quite challenging and does not always lead to a perfect result. Therefore, prevention and early diagnosis and treatment are the best predictors in the treatment of periodontitis
Bone regeneration around teeth with periodontitis
Periodontitis leads to the destruction of the gingiva and of the jaw bone that supports the teeth. During periodontal therapy, most often, although plaque/tartar are removed and the tissues become healthy, the supportive bone around the teeth is not regenerated. In some cases, however, depending on the morphology of the bone defects, the periodontist, using bone grafts and special surgical techniques, can regenerate new supportive bone around the teeth and hence increase their support.
- Initially
- After 12 months (Emdogain)
Periodontitis leads to the destruction of the gingiva and of the jaw bone that supports the teeth. During periodontal therapy, most often, although plaque/tartar are removed and the tissues become healthy, the supportive bone around the teeth is not regenerated. In some cases, however, depending on the morphology of the bone defects, the periodontist, using bone grafts and special surgical techniques, can regenerate new supportive bone around the teeth and hence increase their support.
- Initially
- After 12 months (Emdogain)
Complications of periodontal treatment
Periodontal therapy may have some side effects such as:
- after inflammation is resolved, the gingiva may shrink and: a) the teeth may look longer, b) the roots of the teeth may be exposed, c) spaces between the teeth (black triangles) may form
- after aggressive scaling and root planing, the patient may experience tooth sensitivity to cold stimuli. This sensitivity, although not common, is relieved to a pre-treatment level in a period of 2-3 weeks
Maintaining the effect of the therapy requires meticulous and daily oral hygiene practices by the patient. However, it is not always easy to effectively remove plaque from all surfaces of the teeth, which leads to the recurrence of gingivitis or periodontitis. Periodic re-examinations and professional removal of plaque/tartar from areas with limited access, can prevent the recurrence of the disease.

The interval between two re-examinations is determined based on the patient’s ability to remove the plaque.
The frequency of the recalls is affected also by other factors, such as:
- 1. the severity of periodontal disease
- 2. the number of remaining pockets
- 3. the overall health
- 4. chronic diseases, as diabetes
- 5. smoking and stress
- 6. heredity
- 7. the quality of oral hygiene
- 8. the degree of cooperation with the patient
Periodontal plastic surgery refers to surgical techniques designed to treat periodontal problems that create aesthetic disharmony. These techniques are constantly evolving in modern days and allow, with the help of magnifying glasses and microsurgical tools, the treatment of problems such as the gummy smile, the asymmetry of the gingival margin, the exposure of the roots (recession), etc.
Patients of all ages can benefit from these techniques and improve their smile. So if you’re ready, and you believe you need to change your smile, do not hesitate to contact Dental Group and learn how you can achieve the smile of your dreams. Moreover, apart from the periodontal plastic surgery, the collaboration with qualified and experienced dentists, within the network, specialized in prosthodontics, orthodontics and cosmetic dentistry can further enhance the aesthetic result even in more complex cases.
What is a gingival graft
The gingival graft is a piece of gingiva (gum) suitably positioned to the exposed root surface we want to cover or to a deficient area of the jaw we want to enlarge. The graft is incorporated by the adjacent gums and after a short period becomes as durable as the natural gums.
The main source of a gingival graft is the patient’s palate (roof of the mouth). After taking the graft, the palate heals completely and the patient cannot distinguish the area from which the graft was harvested. However, commercially available grafts are also available and originate from skin tissues, from other donors.
Root coverage
Many times at one or more teeth the gingival tissues recede, exposing part of the root surface. This condition is called gum recession. In this case, apart from the aesthetic problem caused, because the teeth look longer, tooth sensitivity to cold stimuli can develop, as well as an increase of the risk for root caries.
The most common causes of recession are poor oral hygiene, orthodontic tooth movement, intense brushing with a hard toothbrush and the existence of a high frenum.
- Recession caused by poor oral hygiene
- Recession caused by orthodontic teeth movement
- Recession caused by intense brushing with a hard toothbrush
- Recession caused by a high frenum
Whatever the cause of gum recession may be, the problem can be corrected by placing, microsurgically, a gingival graft. Hence, depending on the morphology of the defect, we can predictably cover all or part of the exposed root.
Under local anesthesia a gingival graft is obtained from the palate of the patient and is secured suitably to the root. After 1-2 weeks, the graft is incorporated by the adjacent gums, and it cannot be distinguished from them. In a short period of time the area where the graft was placed, becomes very durable and the patient can brush and chew as if nothing ever happened.
Thus, the aesthetic look of the area is improved, the roots are protected from further recession of the gums, the sensitivity is relieved and the roots are protected from caries. The inconvenience that the patient has during the healing period is very mild and is described by the patients as a mild pulling of the lip.
Case 1
- Before root coverage
- After root coverage
Case 2
- Before root coverage
- After root coverage
Case 3
- Before root coverage
- After root coverage
Case 4
- Before root coverage
- After root coverage
Gιngivectomy
The patient may sometimes notice that the gums are swollen. If the swelling is due to inflammation due to poor oral hygiene, the removal of plaque with the aid of the dentist, restores the gums to their normal dimensions. But there are also cases where the swelling of the gums is due to certain prescribed medicine, as for blood pressure (nifedipine), for epilepsy (phenytoin) or for immunosuppression after transplantation operations (cyclosporine-A). In such cases, the swelling of the gums is fibrous and the only way to remove it, is the surgical removal by applying a technique called gingivectomy.
Gingivectomy is performed under local anesthesia and is limited to the gum tissues without extending into the bone of the jaw. The discomfort the patient endures during the short healing period (1 week) is very mild and is effectively treated with mild pain-killers.
With the procedure of gingivectomy on the one hand, the aesthetics of the gums is restored and on the other hand the ability of applying effective oral hygiene is back. But it should be noted that if the patient continues to take these drugs, the swelling of the gums may recur, so a gingivectomy procedure may be required again in the future.
Case 1
- Before gingivectomy
- After gingivectomy
Case 2
- Before gingivectomy
- Before gingivectomy
Case 3
- Before gingivectomy
- After gingivectomy
Crown lengthening
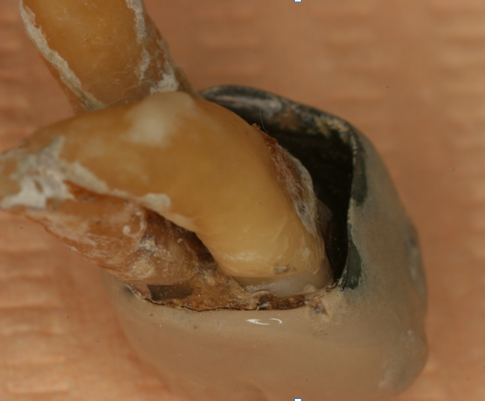
Many times, a tooth may break and its fracture can reach up to the gums. In other cases, there may be cavities in a tooth, which extend below the margin of the gums. In both cases, the restoration of the tooth requires the placement of a crown or a filling. To construct a proper crown or a filling, the borders of the restoration have to be visible and accessible.
For this purpose, by means of microsurgery, the gums and the bone that surrounds the teeth can be repositioned in order to expose the borders of the restoration above the gingival margin. The surgical procedure is called crown lengthening. It is performed under local anesthesia and the discomfort caused by the procedure is similar to the one a patient experiences in a tooth extraction.
Crown lengthening is also done in cases when the teeth are short and we want to lengthen their dimension for aesthetic reasons. In such a case, however, crowns or veneers may be needed to be placed.
- Gummy smile with short teeth
- Before crown lengthening
- After crown lengthening
- After the final restoration
Gummy smile with short teeth
Some people, when smiling, reveal a large part of their gums and their teeth look short and squared. This is because there is excessive gum tissue that covers part of the teeth that normally should be uncovered. Therefore, these teeth, under the gums have a normal shape.
The problem can be resolved by a surgical procedure called crown lengthening and can be applied on one or more teeth. Through this surgical intervention, the excess of gums is removed and the gingival margin is scalloped in such a way as to expose more of the crown of the tooth and thus the tooth appears normal in size and shape.
The result is usually spectacular. The aesthetic appearance is improved and a healthy and attractive smile is obtained. Remarkably, with this technique, because the root of the tooth is not exposed, there is no need to place crowns or veneers to the lengthened teeth. The lengthening of the tooth or teeth is performed under local anesthesia and the discomfort the patient experiences after surgery is similar to the one a patient experiences after a tooth extraction.
- Short and squared teeth
- After crown lengthening
- Final result
Asymmetric smile
The gingival margin of some teeth may be asymmetric leading to an asymmetric smile. In some cases, the technique of crown lengthening may be employed to restore the gingival symmetry and establish a harmonious and symmetrical smile.
However, there are also cases where the problem of asymmetry is due to skeletal problems related to the development of the jaw bone. The treatment of such cases usually requires severe maxillofacial intervention.

Severe asymmetry
due to skeletal problem
Gingival grafts to restore gingival deficiencies
When patients lose several adjacent teeth, then at the edentulous region the gums get flattened. As a result, when large bridges are placed, empty spaces “black triangles” are created between the teeth. Although the result is not always predictable, with the surgical placement of a gingival graft these spaces can be filled. Thus, patients obtain more aesthetic restorations while the troublesome food retention between the teeth gets largely reduced.
- “Black triangles” between the teeth of a bridge
- Almost full coverage of “black triangles” after a gingival graft
Moreover, when a tooth is lost the jaw bone in this region is absorbed, causing the gums to exhibit a “depression” This concavity creates an aesthetic problem to the bridge that will be placed, because the pontic tooth does not appear to emerge through the gums. In addition, this anatomy favors food impaction. With the surgical placement of a gingival graft, it is possible to reverse this negative architecture of the gums and yield a more normal anatomy in the region, restoring cosmetic and oral hygiene problems.
- Gingival concavity under the teeth of a bridge
- Gingival fill after the placement of a gingival graft
Many times, in patients suffering from periodontitis, the teeth migrate forward and open in a shape of a ‘fan’, creating large and unsightly gaps between the teeth. After periodontal treatment and after having fully controlled the inflammation, patients can move their teeth back to their original position with the help of orthodontics. Thus, despite the reduced bone support, the teeth come back into place and the proper occlusion of the teeth is restored. Moreover, the aesthetics get dramatically improved and the new position of the teeth facilitates effective oral hygiene.
Case 1
Before orthodontic treatment
After periodontal and orthodontic treatment
Case 2
- Before treatment
- After periodontal treatment
- After orthodontic treatment
- After restoration or the upper jaw
Today, it is believed that inflammation of the gums can affect the inflammation at the blood vessels and the placenta in two main ways:
- Bacteria from the dental plaque enter the bloodstream and reach the atherosclerotic lesions or the placenta aggravating the pre-existing inflammation.
- Inflammation at the gums causes the development of a systemic inflammation which, in turn, enhances the pre-existing inflammation in atherosclerotic lesions or the placenta.
Therefore, the treatment of periodontitis does not aim in maintaining only the teeth in the mouth, but also the general good health of the patient.
General information
Diabetes mellitus is considered a serious disease where the body does not produce or does not use properly insulin. Insulin is a hormone that the body needs in order to convert sugars into energy, which is necessary in the daily life. Millions of people worldwide suffer from diabetes, and millions of them are also not aware that they are diabetic. If you are aware that you have diabetes, you probably already know, that it is important for diabetics to monitor the progress of their disease and to control the sugar levels through proper diet, exercise or medicines.
However, you may ignore that a good oral health not only prevents inflammations in the oral cavity, but also has a major influence in the control of diabetes.
Diabetes and periodontal disease. A duplex relationship.
Periodontal disease (gingivitis or periodontitis) is an inflammatory disease of the gums and the jaw bone that supports the teeth and is caused by the bacteria of the dental plaque. As with any inflammation in the body, the relationship between periodontal disease and diabetes is characterized as a duplex one.
Diabetic patients appear to have a weaker healing capacity and a reduced ability to resolve inflammation. Thus, these patients are three to four times more likely to develop inflammation at periodontal tissues, in comparison to the non-diabetic patients. Inflammation is usually quite severe in spite of the small amount of plaque. Thus, in diabetic patients the destruction of periodontal tissues is usually quite advanced, and often leads to teeth loss. Moreover, diabetic patients may develop periodically multiple gum abscesses that further destroy the supporting tissues of the teeth.
Simultaneously, periodontal inflammation, as any inflammation of the body, can deregulate the glycemic control and hence aggravate the diabetic condition of the patient. Moreover, teeth loss, due to periodontitis, makes it difficult for the patient to chew and digest food. This is devastating for the diabetic patients, as it affects negatively their ability to ensure good nutrition and hence good control of blood sugar levels.
Diabetes and periodontal treatment
Generally, patients with well-controlled diabetes are treated as non-diabetics. In cases, however, where diabetic control is not satisfactory, the periodontal treatment should be postponed until the blood sugar levels fluctuate to normal or acceptable levels. This is necessary because on the one hand it reduces the risk of the occurrence of a hypoglycaemic episode during the treatment, and on the other hand it increases the possibility of better healing of the periodontal tissue after the treatment, and therefore treatment can be more effective.

Being aware of the patient’s medication and diet, the dentist can determine the ideal time during the day for periodontal treatment. The aim is to avoid the times of the peak action of the insulin, as then the risk of a hypoglycemic episode is increased.
Finally, the diabetic patient has to be aware, that studies have shown that the control of gingival inflammation after periodontal therapy improves the patient’s glycemic control.
General information
Many smokers experience little or no bleeding of the gums and thus they believe they don’t have a periodontal problem. In reality, however, if you smoke or chew tobacco, you have seven times higher chance to develop periodontitis. Additionally, if you are suffering from periodontitis, it usually appears to be more advanced than the one that develops in non-smokers.
Thus, smokers form more tartar on their teeth, have deeper pockets and demonstrate more bone loss around their teeth, as compared to non-smokers. Finally, studies show that smokers lose more teeth than non-smokers due to periodontitis.
How smoking affects periodontitis
The problems caused to the periodontal tissues by tobacco consumption are due to the chemicals contained in the smoke, such as nicotine and tar. Specifically, nicotine constricts blood vessels, resulting in the inadequate blood supply of the gums. This reduces the number of immune cells that enter through the blood circulation in the gingival region and thus impairs the ability to fight the bacteria of dental plaque. For this reason, smokers experience less bleeding of their gums and think that they don’t have periodontitis, when in fact they are the most at risk. Additionally, nicotine adversely affects the immune cells and reduces their ability to recognize, reach and destroy the bacteria of the plaque.

Smoking and periodontal treatment
Smoking adversely affects the healing process of the tissues. Hence, the effect of periodontal therapy, whether it is conservative or surgical, is not always predictable and is inferior to that gained in non-smokers.
Smoking and oral health
Research has shown that smokers, apart from periodontitis, may develop frequently, other problems such as:
- oral cancer
- caries disease
- bad breath
- discoloration of teeth
- stained teeth
- teeth loss
- reduction / loss of taste and smell
- cough

Why is it important to quit smoking
Smoking is recognized as an addiction. Nevertheless, each year millions of people decide to quit. The advantages are many, like reduced chances of developing cancer and lung diseases and also lower costs for medical care.
When quitting smoking, you also have a smaller likelihood your teeth to develop carious lesions and become infected by periodontal disease. Healthy gums are essential to maintain your teeth throughout your life. Last but not least, you should not forget that the oral health affects your overall health.
If you wish to stop smoking, at Dental Group we can guide you through specific smoking cessation programs.
General information
When you are pregnant, you are certainly aware of the importance of taking special care of your body. You ought to acknowledge, though, that pregnancy is a period during which you should take exclusive care of your teeth and gums. The hormonal changes of your body can make your gums more susceptible to the harmful dental plaque that forms on the surface of the teeth and thus the probability of developing gingivitis is increased. Furthermore, if you already have symptoms of gingivitis, the inflammation may exacerbate during pregnancy.

When you are pregnant, you are certainly aware of the importance of taking special care of your body. You ought to acknowledge, though, that pregnancy is a period during which you should take exclusive care of your teeth and gums. The hormonal changes of your body can make your gums more susceptible to the harmful dental plaque that forms on the surface of the teeth and thus the probability of developing gingivitis is increased. Furthermore, if you already have symptoms of gingivitis, the inflammation may exacerbate during pregnancy.
What are the symptoms of gingivitis during pregnancy
Approximately 70% of women suffer from some form of gingivitis during pregnancy. There are some warning signs about the presence of gingivitis that you shouldn’t ignore:
- the gums are sensitive, swollen or red
- the gums bleed while brushing or flossing
- bad breath (halitosis)
If you notice any of these symptoms, you should visit the dentist for an oral examination and a professional cleaning.
Additionally, in some cases pregnant woman may develop a gingival enlargement, like an abscess, in a small area of the gums that is called pregnancy epulis. The epulis usually subsides right after pregnancy. However, if it does not subside or if it creates difficulty while chewing or aesthetic issues during pregnancy, it can be removed with a small and painless gingivectomy procedure.

Association of periodontal disease with pregnancy complications
Since the 1990s a large number of studies have been conducted in order to investigate the possible correlation between periodontal disease and pregnancy complications (premature and underweight babies, preeclampsia, miscarriage, gestational diabetes mellitus). By these studies the scientific community has been led to the conclusion that gingivitis and periodontitis increase the risk of preeclampsia during pregnancy. However, the treatment of gingivitis and periodontitis during pregnancy does not appear to prevent adverse pregnancy outcomes. It is possible that the biological processes that contribute to the occurrence of pregnancy complications have initiated before the completion of the periodontal treatment and the damage is irreversible. Therefore, periodontal therapy may be better to occur, prior to pregnancy.
Cardiovascular diseases and periodontal therapy
Many patients suffer from various cardiovascular diseases such as angina, heart attack, stroke, hypertension, heart failure, heart arhythmias, etc. The dentist should be informed by the patient for all of these diseases in detail, in order for the dentist to be able to protect the patient from unpleasant complications. Thus, patients suffering from the following health problems should not receive dental treatment, unless this is absolutely necessary and always after consulting with their physician:
- unstable angina
- recent heart attack, in less than the last six months
- recent stroke, in less than the last six months
- vascular grafts that have been placed in less than a month period
- uncontrolled high blood pressure (> 210/120 mmHg)
Furthermore, patients who follow a prescription of anticoagulants medicine may need to modify their treatment during periodontal therapy or teeth extractions.
Moreover, some medications for high blood pressure can cause gingival enlargement and thus create an aesthetic problem and difficulty in oral hygiene performance.

Finally, in cases of risk for endocarditis, the patient may need to take antibiotics before the dental treatment.
In any case, the dentist, in cooperation with the patient’s cardiologist, may alter the treatment and the drugs taken by the patient, in order to perform the dental treatment in the safest way.
Association of periodontitis with cardiovascular diseases
Since the 1990s a large number of studies have been conducted investigating the possible association between periodontal disease and cardiovascular disease (heart attack and stroke). Through these studies, the scientific community has been led to the conclusion that periodontitis increases the risk of a heart attack and a stroke. This risk is higher for stroke.
Periodontal bacteria have been detected in atherosclerotic lesions, while in periodontal patients atherosclerotic plaques are more unstable. This causes atherosclerotic plaques to be more prone to develop an infarct and hence, an ischemic episode.